Having a major clear out (again). Stuff in the loft in our old house packed up, moved up north (after several months in storage) and stored in a big old cupboard here in Buxton for four more years.
This work is inevitably charged. Small stories fallen into cardboard box cracks, separate from curated childhood memories. Lego pieces, Playmobile accessories, torn ticket stubs, photos that didn’t make the album cut, newspaper cuttings. Unexpected chuckles, breath-stealing sadness.
It needs sorting because the sentimental value of objects, of stuff, doesn’t necessarily translate. Story/memory-making happens around and beyond things, anchoring them in time and places that aren’t always apparent.
A Chatsworth car park ticket. Peak District holiday as pups. Our dad parked on a grass verge next to a ‘No Parking’ sign the size of the house he wanted to film. He took his camera out of the boot and locked the car keys in it. Oh my childhood days. Waiting, waiting, waiting. The day derailed with awkwardness. Handstands and cartwheels. Passing drivers clearly marking the rule breach. A policeman finally pitched up with a biscuit tin of metal car keys to release us. So much more than a parking ticket.
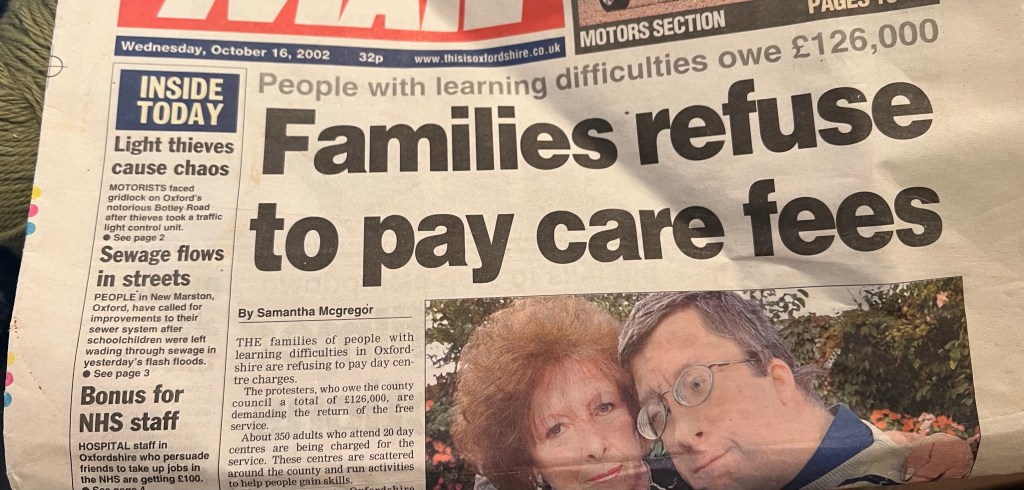
Some stuff does speak for itself. Protest and protests. Reported, repeated dated events.

A Guardian Society piece from 2003. Donal MacIntyre arguing for a home assault law to recognise that ‘the deprivation of social contact, denial of food, medicine and care, and infliction of petty humiliations and degradations can constitute abuse and should be liable to prosecution’. He describes the newly created Commission for Social Care Inspection (CCSI) as ‘the future but unless it determinedly disassociates itself from previous passivity, then little will change’.
Prophet Donal. Pre-CQC, Winterbourne View and so much more.
Letters I’d forgotten writing.
Hey, Anneliese Dodds MP, what’s going on with the woeful progress of the Leder programme? (Always receipts when you throw nothing away). Prof Stephen Powis, NHS England, typed the type here. Delays, failings and always more to do.
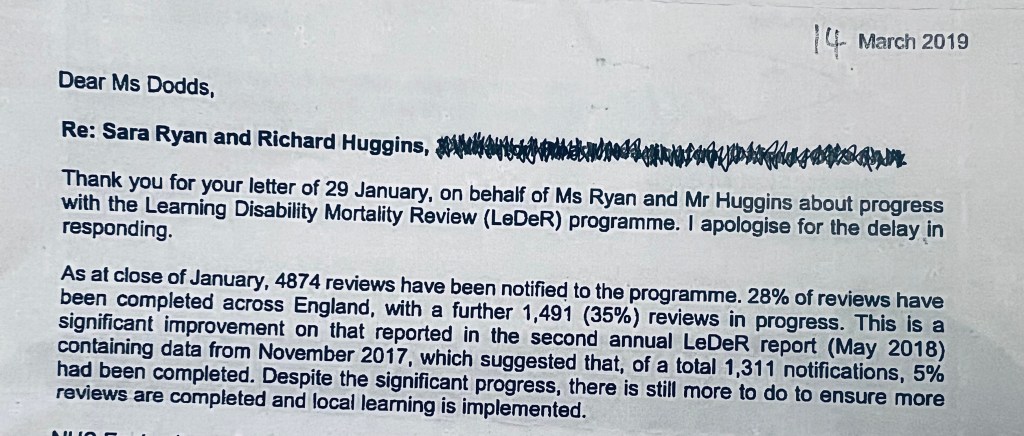
Where’s Prof Powis now? Does he remember writing these words, defending the indefensible, and putting his name to them? What remains of the Leder review seven years on is the stuff of dogs dinners.
Finally, our Michael. Michael Edwards. President of My Life My Choice. An article I cut out and kept when Connor was walking on Welsh beaches without an inspectorate, quality, standards commission care in the world.
Michael tells the story about sorting plastics in an Oxford centre.
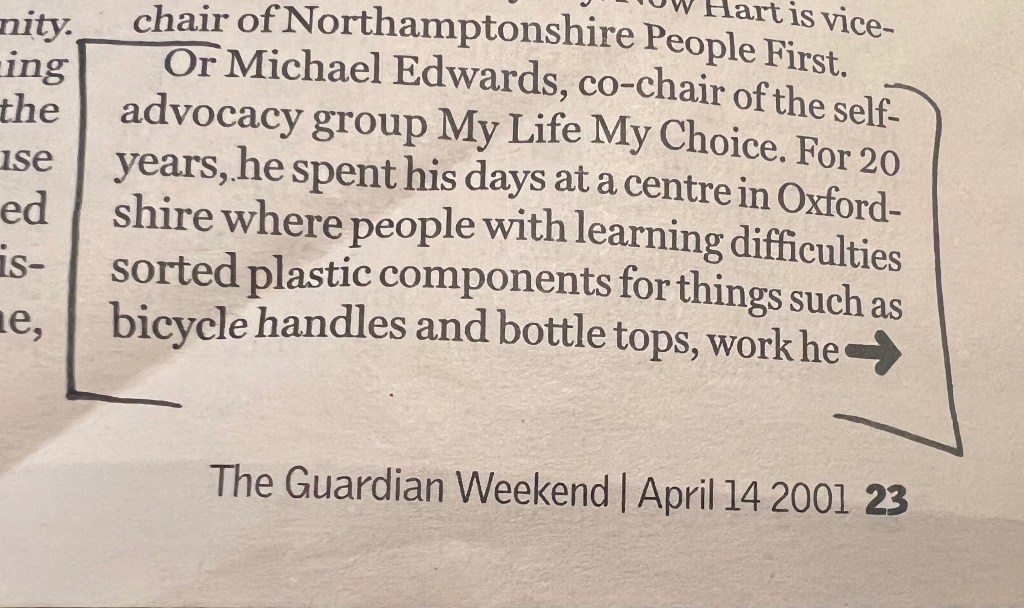
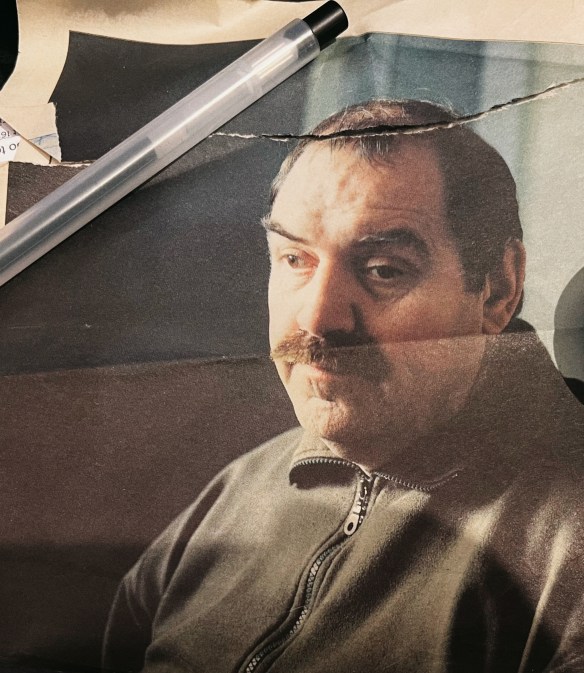
I marked these sections back in the day before I met Michael and My Life My Choice. Reading about the mixing up of plastics cut me to the core before I had the words or even thoughts to make sense of it. Oddly, rightly, this article was instrumental in me getting in touch with My Life My Choice a few years later when I had my first research job. Eventually developing a relationship of friendships, love, laughter, care, commitment, collaboration and activism. Something I treasure beyond words.
It doesn’t take much to join the dots between these stories plotted from randomly stored stuff. People involved/implicated and then absent. Exposing, reporting, ‘leading’, deflecting with little or no sustained thought for the people and their families harmed by these enduring abuses. People who continue to resist and stand taller than that ‘no parking’ sign from back in the day.